A 10-year multidisciplinary collaboration across three Australian universities has resulted in the development of a water-based gel that improves the survival of cell transplants. In preclinical trials, the gel repaired damaged mouse brains.
One in six people will be affected by brain disease and disorders in their lifetime, The Brain Foundation estimates.
No current treatment can reverse the effects of neurological diseases, so much research and development focuses on finding drugs to slow or stop their progression.
“We are focused on developing stem cell-based neural grafts to promote brain repair,” says neurologist and stem cell biologist Professor Clare Parish.
Cell therapies could be particularly powerful in conditions like Parkinson’s disease where small, discrete populations of cells are affected. But treating more extensive brain damage, for example caused by stroke, is more complicated.
“The challenges here include getting the right cell type – or types – in sufficient supply to stay in the brain when there is a large void in the brain caused by the stroke,” Professor Parish says.
A material that improves cell survival in cell therapies
A team of researchers across the University of Melbourne, Australian National University (ANU), Deakin University and the Florey have developed a solution.
“The material provides a safe sanctuary environment for those cells, and improves the survival about fourfold,” says Professor David Nisbet from the University of Melbourne’s Faculty of Engineering and IT.
The material, a water-based gel or hydrogel, improves stem cell grafts by:
- Protecting cells in the syringe during administration
- Supporting the newly transplanted cells to ‘knit’ into the brain
- Promoting the cells’ survival by supplying additional oxygen.
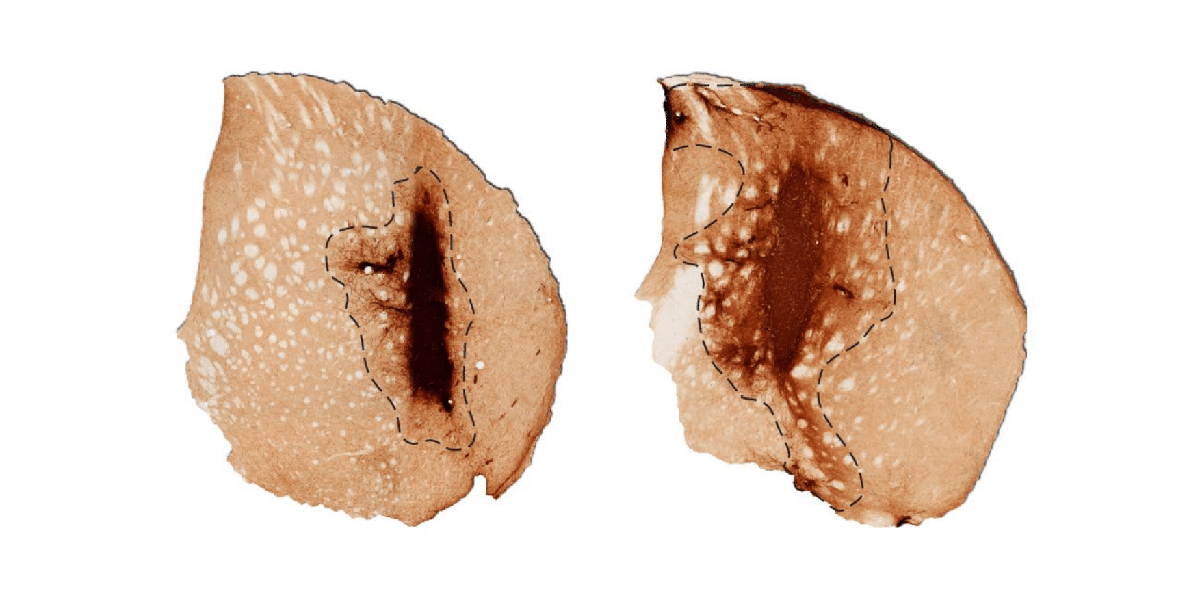
The hydrogel successfully repaired injured mouse brain tissue in pre-clinical trials published in Nature Communications.
Although these results are promising, this technology still has many years of development ahead before it may become available for human patients. The team is seeking an industry partner with whom to begin Phase I clinical trials. Meanwhile, they continue to work on adapting the hydrogel for other cell transplantation techniques.
“We’ve got a whole suite of different materials with different amino acid sequences, structures and properties,” Professor Nisbet says.
A PCT patent application for the hydrogel was filed jointly by the University of Melbourne, ANU, Deakin University and the Florey in 2023.
Subscribe to our MedTech newsletter
Interdisciplinary collaboration powers innovation
“It’s 10 years of work coming into fruition at the moment,” Professor Nisbet says.
Professor Nisbet is a biomedical engineer and leads the project at the University of Melbourne. His collaborations with Deakin’s Associate Professor Richard Williams, the Florey’s Professor Clare Parish and ANU’s Professor Colin Jackson have powered the material’s development.
“Richard's a materials scientist. Clare's a stem cell biologist, a neuroscientist. Colin's a protein engineer. And I suppose I'm probably a hybrid of them all,” Professor Nisbet says.
Associate Professor Williams and Professor Nisbet together designed a way to make small fragments of protein come together and form nanofibers, which would then self-assemble into a hydrogel. As a materials scientist, Associate Professor Williams’ contribution is in fine-tuning the physical properties of the material to deliver the subtle signals that are required by the biologists to control cell behaviour.
“We used to meet up after work to ride bikes together. … And then we started chatting to each other about our work,” Associate Professor Williams says.
“It shows that the seeds of innovation find fertile ground in these small conversations.”
Professor Parish is a long-time colleague and collaborator of Professor Nisbet’s. She provides insight into cellular and brain biology, and her lab at the Florey – the largest brain research centre in the Southern Hemisphere – conducts all in vivo testing on the hydrogel.
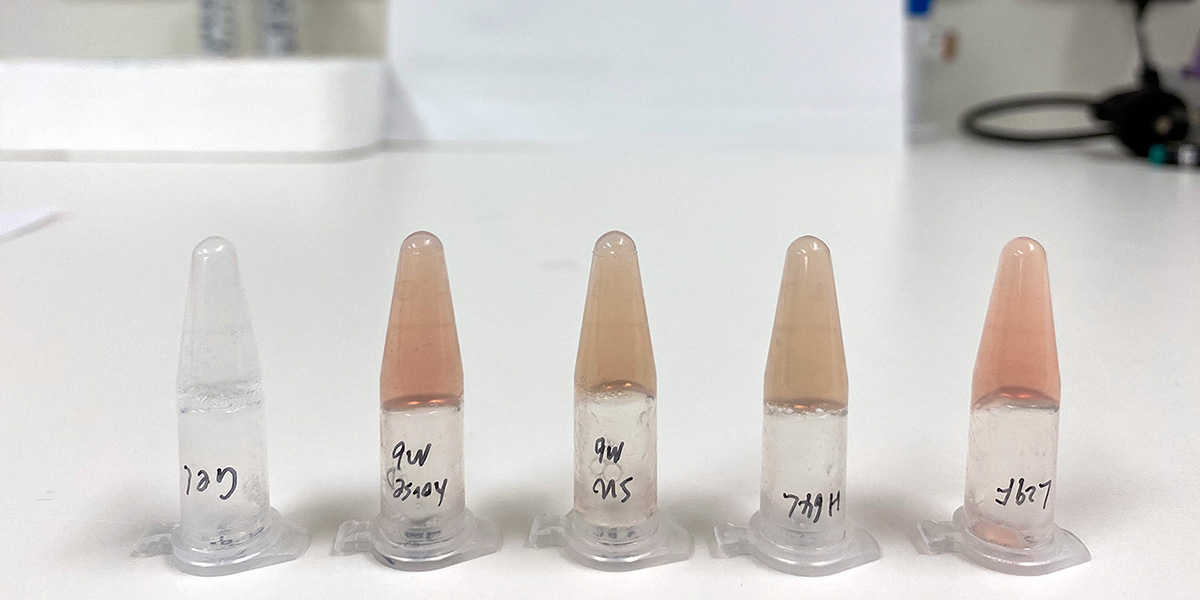
The synthetic blood system that has boosted the performance of grafts using the hydrogel, especially for large dead areas of cells, was developed with Professor Colin Jackson. The blood system is a synthetic protein based on myoglobin, a protein which delivers oxygen to the muscles of horses and whales.
“I’m involved in every single aspect of the project,” Professor Nisbet says.
Working across multiple leading Australian universities gives the team access to more research infrastructure, as well as access to a diverse pool of experts for problem-solving.
“If we haven’t got something in an individual university, one of the collaborator universities will have it,” Associate Professor Williams says.
The collaborators agree the mixture of different disciplines has been crucial in driving innovation, and that without interdisciplinary collaboration, research can become trapped in siloes – whether that’s protein chemistry or neurology.
“There's no point collaborating with somebody who can just do what I can do,” Professor Nisbet says.
“For any young academics who are just starting out, forming a resilient network across institutions is a vital thing if you want to develop really impactful research output,” Associate Professor Williams says.
First published on 15 July 2024.
Share this article
Keep reading
-
Explore more MedTech research
Creating transformative solutions for patient treatment and recovery. We bring together expertise from engineering, technology, medicine and science to develop tools to improve community health and individual patient outcomes.
-
Partnerships
Find out how we can help to grow your organisation - from talent, to projects and partnerships.
-
Torch Recruit: bringing clinical trials to regional patients
The University of Melbourne is collaborating with regional and rural GPs across the country to improve health outcomes, with the help of an innovative new platform.
-
Improving quality of life through biomechanics, surgery and industry collaboration
Melbourne-based start-up MAXONIQ has developed a break-through, 3D-printed jaw for debilitating end-stage bone and joint conditions, improving the lives of patients worldwide.