Doctors and parents sometimes disagree about the best medical treatment for a child. The Zone of Parental Discretion helps healthcare professionals navigate decision-making with families.
4 Minute read
The outcome
Health professionals now have a tool to help them reach an ethical resolution when parents and doctors disagree about the medical treatment of a child.
The Zone of Parental Discretion (ZPD) tool comprises five questions that help doctors make ethically informed decisions. The questions consider harm that might arise from a parent's decision, as well as harm from overriding a parent's decision.
The tool describes when parents can make decisions about their child’s healthcare, even if the decision might not lead to the best possible outcome for the child. The tool aims to:
- balance children’s wellbeing with parents’ rights to make medical decisions for their child
- ease the distress that disagreements over treatment can cause for both doctors and parents
- resolve conflicts around care while protecting the health rights of children.
The tool was developed by Professor Lynn Gillam, Dr Rosalind McDougall and Professor Clare Delany from the Children’s Bioethics Centre at the Royal Children’s Hospital in Melbourne.
The research team has since developed the tool into a book, When doctors and parents disagree: Ethics, paediatrics & the zone of parental discretion. The book offers ethical and practical guidance based on real-life cases. The tool is used in Australia and internationally in clinical and education settings.
The need
When a child is ill, parents and doctors usually agree on the appropriate medical treatment. But sometimes, parents and doctors disagree. Parents might want to try a treatment that doctors think has a limited chance of success. Doctors might recommend a treatment that parents worry will cause serious side effects for their child.
When deciding how best to respond to a parent that disagrees with their recommendation, doctors typically consider the child’s best interests. This includes:
- appropriate medical treatment
- family and social situation
- long-term wellbeing
- treatments that limit harm to the patient and their family.
But researchers had found from clinical experience that it is not always possible to determine what is ‘best’. There may be competing views that cannot be resolved. Or there may be a lack of clear evidence on which treatment is likely to produce positive results. And this approach can disregard the parents’ autonomy.
While these ethical cases are rare, they can cause distress to the child, their family and medical staff. They may cost more time and money to resolve, which could negatively affect treatment and the healthcare system. Healthcare professionals needed more robust ethical and practical guidance to help them navigate these situations.
Developing the solution
The concept of the zone of parental discretion arose from the team’s experience providing clinical ethics guidance at the Royal Children’s Hospital. Since the Children’s Bioethics Centre was launched in 2005, the staff at the Centre have provided ethics guidance on more than 180 clinical cases. Around 22 per cent of these involve situations where parents disagree with doctors’ recommendations.
For example, parents of children with cancer might decline conventional treatment in favour of alternative therapies. Or refuse a blood transfusion on religious grounds.
The research team examined these cases and considered questions such as: why are the parents disagreeing with doctors, and what would happen to the child if the treatment was not given?
Using common features of these cases, the team developed the tool as a two-step approach. First, it helps doctors understand the parents’ decision, and determine whether it could cause harm to the child. Second, it helps doctors assess whether overriding the parents’ decision could negatively affect the child. Doctors also need to consider whether those negative effects would be worse than the harm caused by accepting the parents’ request.
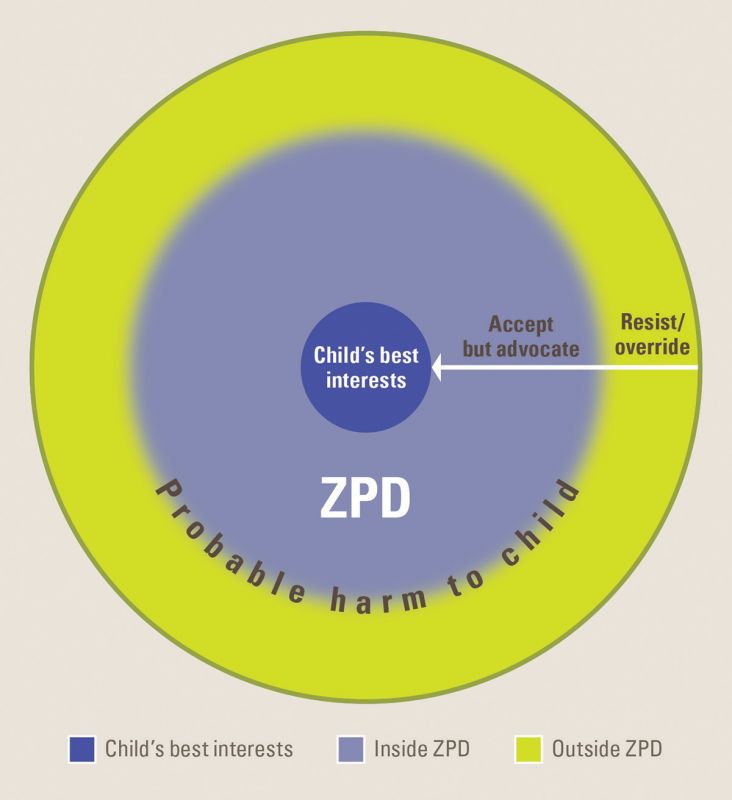
The tool helps doctors identify when it is ethical to override a parent’s choice. For example, should doctors accept a treatment option that parents want, providing it is ‘good enough’, rather than insisting on the ‘best possible’ treatment. This might happen when parents want a form of surgery that isn’t the best available but may still treat their child’s condition.
The tool includes five questions:
- What are the parents’ wishes or decision?
- What would be the effects on the child of carrying out the decision?
- Are these effects so bad as to constitute probable significant harm to the child?
- What would be the effects on the child of attempting to or succeeding in resisting or overriding the parents’ decision?
- If there are likely to be negative effects on the child, would this constitute greater harm to the child than the harm expected from the parents’ original decision?
To help healthcare professionals use the tool, the team compiled When doctors and parents disagree: Ethics, paediatrics & the zone of parental discretion. The book uses anonymised ethical situations based on actual cases, to show how the Zone of Parental Discretion can be used to resolve disagreements.
The Zone of Parental Discretion tool can be used alongside other ethical tools such as the Charter on the Rights of Children and Young People in Healthcare Services in Australia. The Charter provides a framework to help children and young people know about their rights, and ensure they receive healthcare suitable for both them and their families. The Charter was created with the involvement of researchers from the Children’s Bioethics Centre, in collaboration with Children’s Healthcare Australasia and the Association for the Wellbeing of Children in Healthcare.
Partners
The Royal Children's Hospital Melbourne
Funding
ARC Discovery Early Career Researcher Award
When should health professionals override parents' decisions about a child's medical treatment? (DE120100488)
Publications
Gillam L (2016) The zone of parental discretion: An ethical tool for dealing with disagreement between parents and doctors about medical treatment for a child. Clinical Ethics 11(1): 1–8. doi: 10.1177/1477750915622033
McDougall R, Delany C, Gillam L (eds; 2016) When doctors and parents disagree: Ethics, paediatrics & the zone of parental discretion. Sydney, Australia: Federation Press. ISBN-13: 9781760020590
Re-use this text
Please use the text of this article for your own purposes. The text is licensed under the Creative Commons Attribution (CC BY) 4.0 International license. This lets you copy, transform and share the text without restriction. We appreciate appropriate credit and links back to this website. Other content on this page (such as images, videos and logos) is not covered by the CC BY license and may not be used without permission from the copyright holder. If you have any questions about using this text, please contact the research web team.
First published on 2 March 2022.
Share this article
Keep reading
-
Pursuit: The ethics of a child’s future fertility
Chemotherapy can leave young patients infertile; a University of Melbourne bioethicist has created the world’s first ethical framework for decision-making about a child’s future fertility.
-
The Conversation: When parents disagree with doctors on a child’s treatment, who should have the final say?
As the recent case of six-year-old boy Oshin Kiszko highlights, some disagreements between doctors and parents can’t be resolved by further information and discussion.
-
ABC Radio National: Hospital ethics
What happens when doctors and ethicists get together – particularly when the patient under discussion is a young child? And how can philosophy help?
-
Child and Adolescent Health PhD Program
Join our Child and Adolescent Health PhD Program and work with other graduate researchers from the Melbourne Children's Campus.